Introduction: Various studies have shown that Black and certain minority patients with hematologic malignancies have worse survival outcomes than White patients in the United States. In the current study, we compared the survival outcomes of Non-Hispanic Black (NHB), Hispanic, and NH Asian/Pacific Islander (API) to Non-Hispanic White (NHW) across different types of hematologic malignancies in multiple different healthcare settings.
Methods: We identified adult patients with newly diagnosed lymphoma, myeloma, or leukemia from 2011-2020 in Surveillance, Epidemiology, and End Results Program (SEER), as well as respective cancer registries linked to electronic data warehouses at Veterans Affairs (VA) national healthcare system and Harris Health System (HHS). VA is a unique single-payer system with patients covered by veteran benefits. HHS is a large safety-net county hospital system in the Houston metropolitan area with >80% of uninsured and charity care. These hospital systems were chosen to represent opposite ends of the spectrum of healthcare access; however, we explicitly chose not to compare survival outcomes across institutions due to inherent differences. For each patient cohort, we built unadjusted and adjusted multivariable Cox regression models to assess the impact of race/ethnicity on overall survival. The adjusted factors included age, sex, marital status, rurality, median household income, diagnosis year, cancer histologic subtype, and cancer stage (for lymphoma). Type and time to treatment were not included as these were associated with access to care. In a sensitivity analysis, we also included NCI comorbidity index and ECOG performance status (PS) in VA and HHS (not available in SEER).
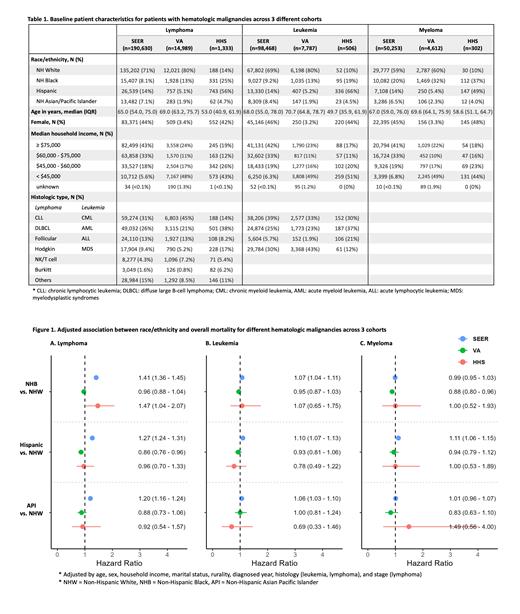
Results: Patient characteristics from the 3 cohorts are shown in Table 1. SEER patients (n=339,351) were more representative of the US census (71% NHW, 14% Hispanic, 8% NHB, 7% API). In contrast, VA patients (n=27,388) were mostly male (97%) with lower median income ($45,000) and with more NHB (16%); HHS patients (n=2,141) were notably younger (median 53) with lower median income ($47,409) and more Hispanic (57%) and NHB (25%). On unadjusted analysis, significant variables associated with mortality in all cohorts included older age, male sex, lower income, aggressive histology, advanced stage, higher PS, and more comorbidities. Race/ethnicity had variable association with mortality depending on the healthcare setting.
On multivariable analysis adjusted for other confounders (Figure 1), race/ethnicity continued to exhibit variable association with overall mortality depending on cancer type and healthcare setting. Across all cancers, minority groups had similar or worse adjusted survivals than NHW in SEER, while they had similar or better adjusted survivals than NHW in VA. With exception of NHB vs. NHW in lymphoma, minority groups had no significant differences than NHW in HHS.
Since both VA and HHS were enriched with NHB patients, we next focused on the comparison between NHB vs. NHW. For lymphoma, the adjusted hazard ratio (HR) for mortality was 1.41 (95% CI 1.36-1.45), 1.47 (95% CI 1.04-2.07), and 0.96 (95% CI 0.88-1.04) in SEER, HHS, and VA, respectively. For leukemia, the adjusted HR was 1.07 (95% CI 1.04-1.11), 1.07 (95% CI 0.65-1.75), and 0.95 (95% CI 0.87-1.03) in SEER, HHS, and VA, respectively. For myeloma, the adjusted HR was 0.99 (95% CI 0.95-1.03), 1.00 (95% CI 0.52-1.93), and 0.88 (95% CI 0.80-0.96) in SEER, HHS, and VA, respectively. The other minority groups followed a similar trend. In the sensitivity analysis where ECOG PS and NCI comorbidity index were included for HHS and VA, the overall observations by race/ethnicity were not significantly different. In additional subgroup analyses limited to older patients or males, the overall finding was also not different.
Conclusions: In summary, racial/ethnic disparity persists at-large in the US (SEER) for most hematologic malignancies, even after accounting for cancer-, patient-, and socioeconomic factors. However, minority status has neutral or protective effect vs. NHW in healthcare system without barrier to access (VA), while its impact appears similar to the national trend in healthcare system with significant barriers to access due to the lack of insurance (HHS). Healthcare access may contribute to the ongoing racial/ethnic disparity for survival outcomes observed in hematologic malignancies in the US.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal